- All posts
- 8 Media Venture
- althetics
- aMMP8
- Annimari Korte
- Antibiotic resistance
- Apotek Härtat
- Aqua Dental
- athlete
- Award
- Baltics
- Bonnier
- Bonnier News
- Brain health
- Business
- Cancer
- cardiovascular disease
- caries
- Chemo therapy
- children
- collaboration agreement
- Croatia
- Denmark
- Denta
- Dental erosion
- Dentex
- diabetes
- Dual Light
- Duodecim
- EFP
- EFR
- Estonia
- EuroPerio
- event
- Expodental
- FIBO
- fund raising
- general health
- Gingivitis
- Gum disease
- HAP
- HealthHub Pharma
- HIDES
- Hospital infections
- hospital-acquired pneumonia
- IBD
- Iceland
- IDS COLOGNE
- implantology
- invest
- investment
- italy
- Koite Health
- Latvia
- Lithuania
- lumoral
- Lumoral App
- Lumoral Junior
- Maritime industry
- Media
- MegaGen
- Movie
- News
- Nordic markets
- Nordics
- O
- Olympics
- Oral health
- Oral hygiene
- Oral mucositis
- Patent
- PDT
- peri-implantitis
- Perio Master Clinic
- Periodontitis
- periodontology
- Photodynamic therapy
- Press
- Ranking
- Romania
- Scandinavian Society of Periodontology
- Science
- Seafarer
- Seedtable
- share issue
- Shareissue
- Siblings movie
- Spain
- spots
- Stroke
- Study
- sweden
- Tartar
- techtour
- Thailand
- UK
- United States
- Valentine's Day
- WHO
- World Cancer Day
- World Health Day
- World Heart Day
- world oral health day
- World Smile Day
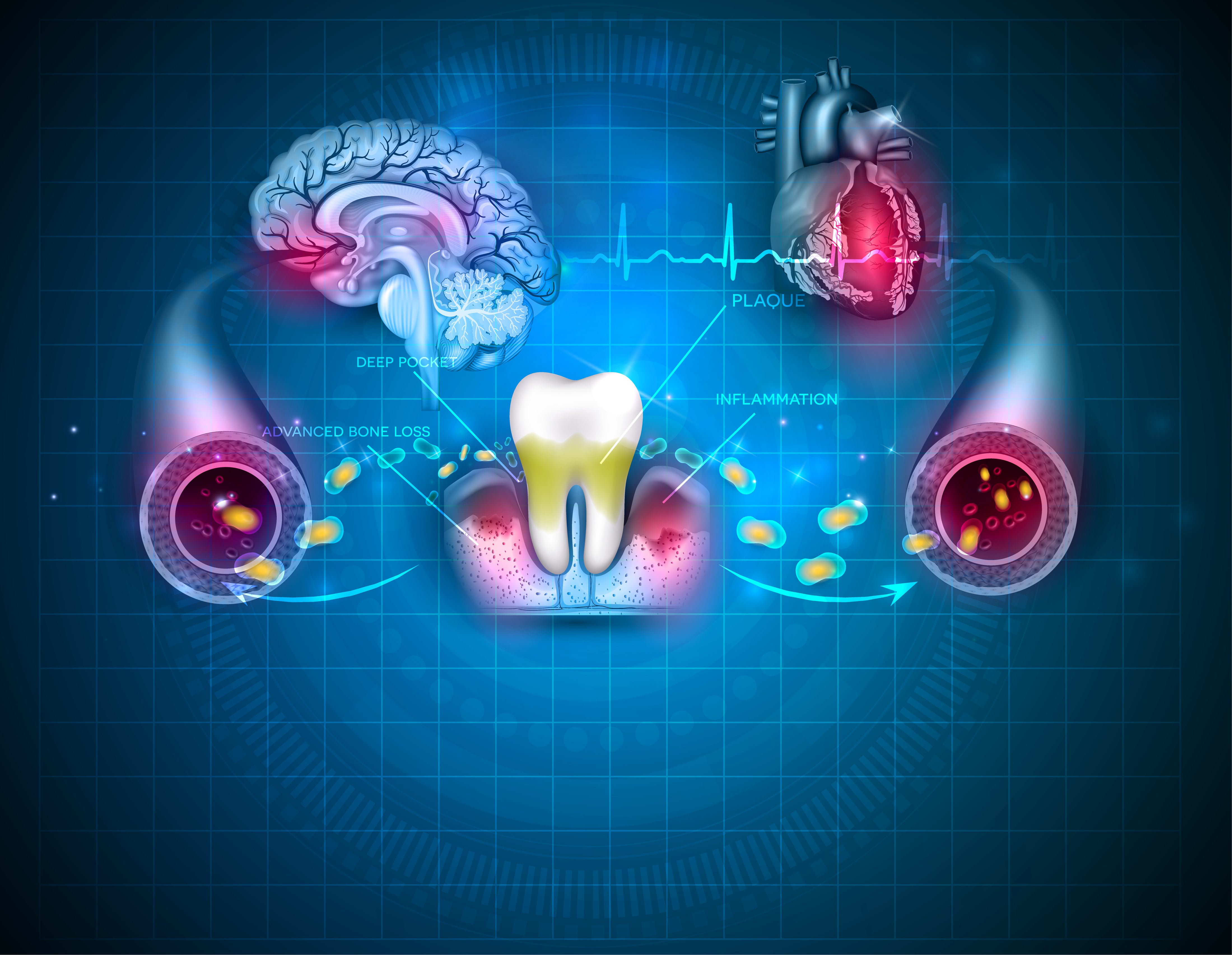
The mouth is a gateway to infection in the body
Good oral hygiene is an essential part of the basic management of kidney and liver disease. For transplant patients, oral health care is particularly important as these patients are often at increa...
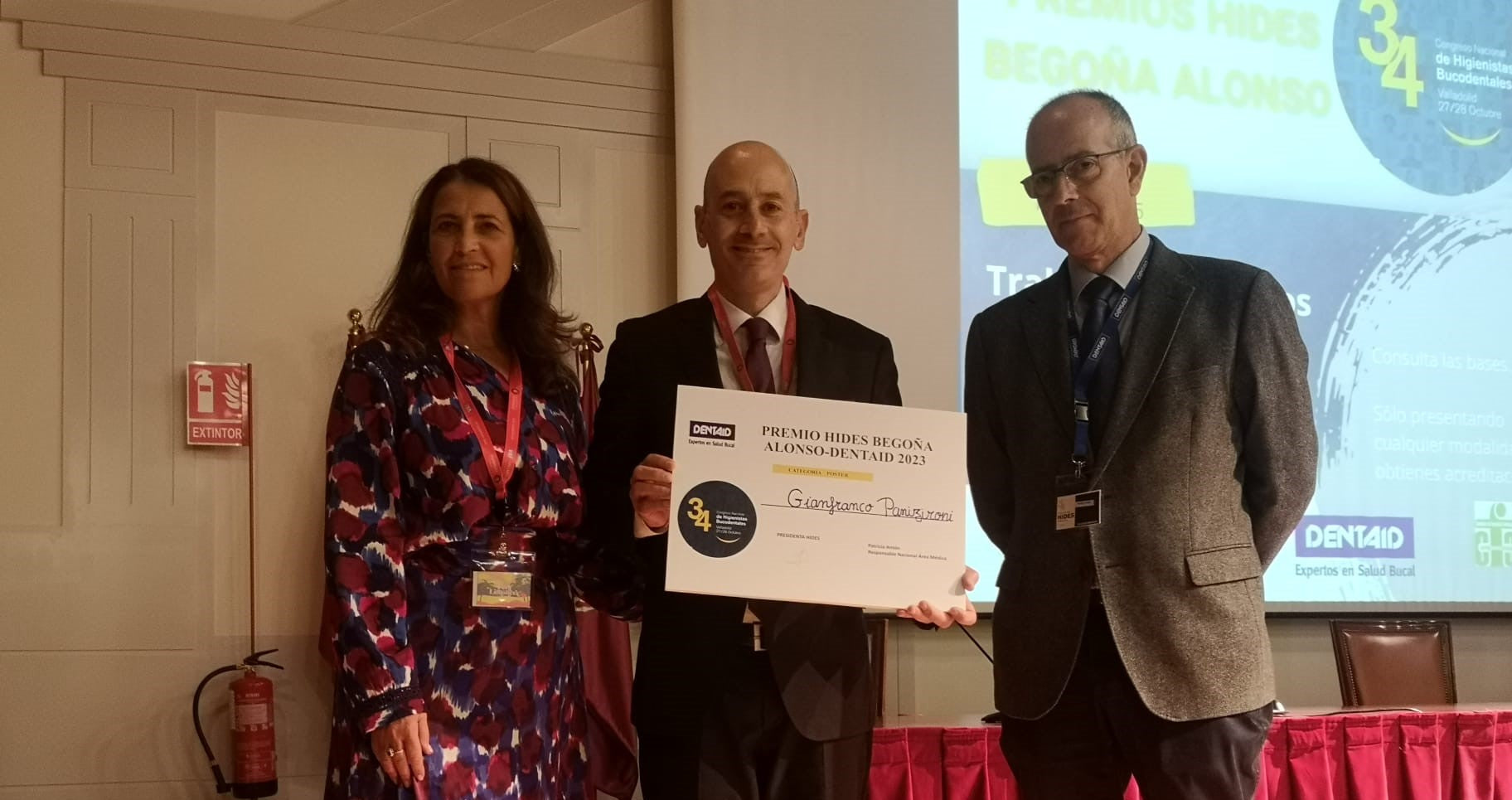
HIDES 34th National Congress in Spain Acknowledges Award-Winning Lumoral Study Poster
On October 27th and 28th, the Spanish Federation of Dental Hygienists (HIDES) hosted its 34th National Congress in Valladolid, Spain. The event attracted around 300 attendees, including dental hygi...

A healthy mouth is a prerequisite for successful implant treatment
Finland is a rather conservative country when it comes to dental implant treatments. Unlike in many other European countries, where demand for implants is growing strongly as the population ages, t...

Finland’s Koite Health partners up with a major player in the Italian implant industry
Finnish health technology company Koite Health has signed a distribution accord with Megagen Italia, which markets cutting-edge dental implant systems and advanced surgical devices. As a kickoff to...

Periodontitis, or severe gingivitis, is a common disease that is estimated to affect about 20-50% of the global population – often without any symptoms at all. Now, for the first time, a Finnish st...
Lumoral's journey from a brilliant idea to a unique oral health medical device
Koite Health Oy is a Finnish health technology company that develops light-activated antibacterial solutions for the treatment and prevention of oral diseases. The company’s Lumoral teeth cleaning ...