- All posts
- 8 Media Venture
- althetics
- aMMP8
- Annimari Korte
- Antibiotic resistance
- Apotek Härtat
- Aqua Dental
- athlete
- Award
- Baltics
- Bonnier
- Bonnier News
- Brain health
- Business
- Cancer
- cardiovascular disease
- caries
- Chemo therapy
- children
- collaboration agreement
- Croatia
- Denmark
- Denta
- Dental erosion
- Dentex
- diabetes
- Dual Light
- Duodecim
- EFP
- EFR
- Estonia
- EuroPerio
- event
- Expodental
- FIBO
- fund raising
- general health
- Gingivitis
- Gum disease
- HAP
- HealthHub Pharma
- HIDES
- Hospital infections
- hospital-acquired pneumonia
- IBD
- Iceland
- IDS COLOGNE
- implantology
- invest
- investment
- italy
- Koite Health
- Latvia
- Lithuania
- lumoral
- Lumoral App
- Lumoral Junior
- Maritime industry
- Media
- MegaGen
- Movie
- News
- Nordic markets
- Nordics
- O
- Olympics
- Oral health
- Oral hygiene
- Oral mucositis
- Patent
- PDT
- peri-implantitis
- Perio Master Clinic
- Periodontitis
- periodontology
- Photodynamic therapy
- Press
- Ranking
- Romania
- Scandinavian Society of Periodontology
- Science
- Seafarer
- Seedtable
- share issue
- Shareissue
- Siblings movie
- Spain
- spots
- Stroke
- Study
- sweden
- Tartar
- techtour
- Thailand
- UK
- United States
- Valentine's Day
- WHO
- World Cancer Day
- World Health Day
- World Heart Day
- world oral health day
- World Smile Day

Periodontitis and Diabetes: The Connection Between Two Common Diseases
Periodontitis and diabetes are two prevalent diseases with a strong bidirectional relationship between them. Poorly managed diabetes promotes the progression of periodontitis and complicates its tr...
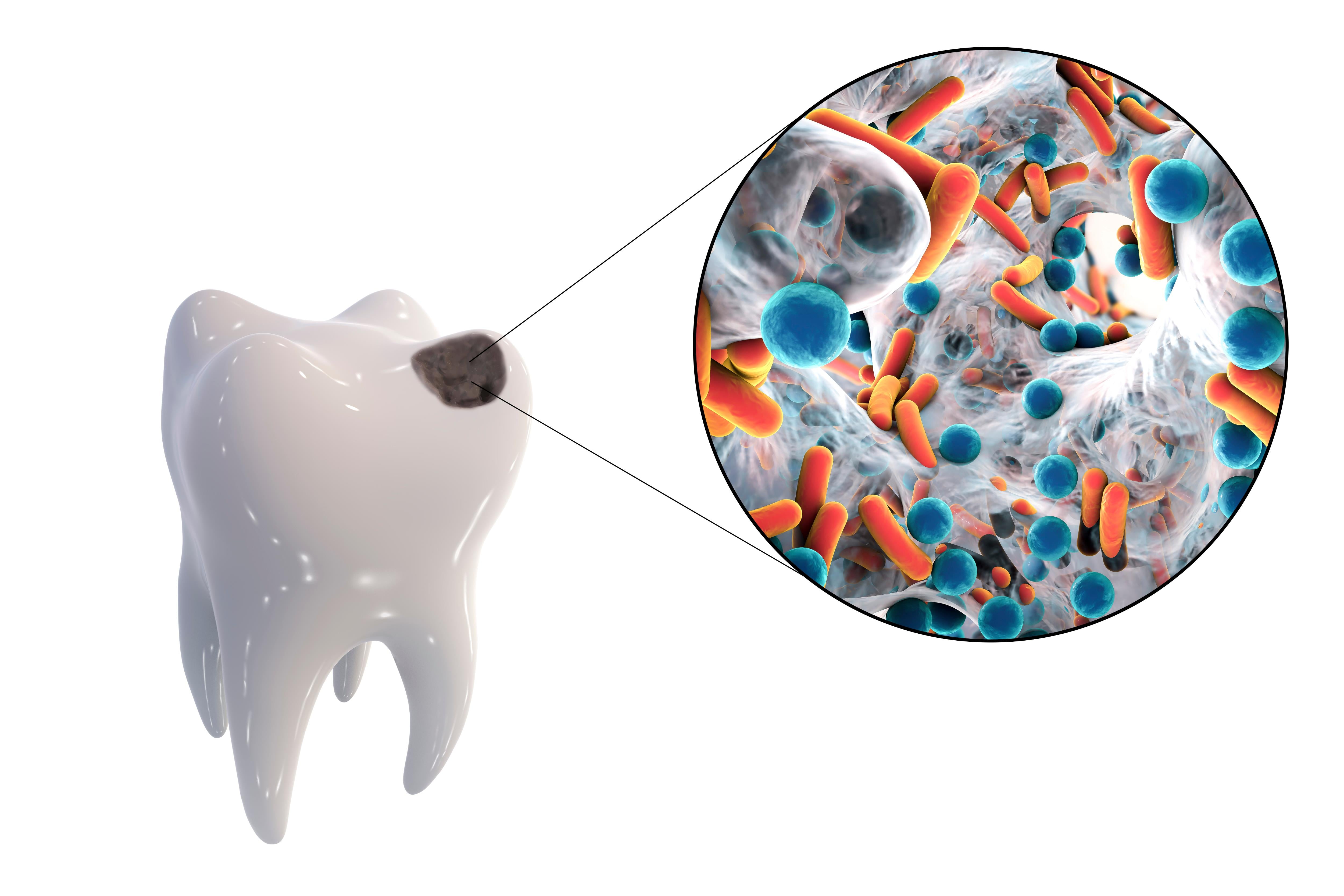
According to a report commissioned by the European Federation of Periodontology (EFP), 4.9 percent of global healthcare expenditure is allocated to treat preventable oral diseases such as gum infla...

Good oral health supports seniors' overall health - International Day of Older Persons on 1 October
Maintaining good oral hygiene and oral health is paramount for overall well-being. When it comes to older individuals, proper dental care goes beyond just addressing oral issues; it also plays a cr...

World Oral Health Day reminds us of the link between oral and general health
World Oral Health Day is celebrated annually on 20 March to raise awareness of good oral hygiene and its link with general health. Special attention to the importance of oral health is needed at th...

Strong link found between tooth loss and inflammatory bowel disease
Inflammatory bowel disease is linked to an increased risk of periodontitis, i.e. periodontal disease. This is according to new publications from a European research project that explored the link b...

WHO: Oral health is a key indicator of overall health, well-being, and quality of life
Why is oral health so important for everyone? The mouth is the “starting point” of the body’s defense and immunity system. When oral health is compromised by disease or injury, general health is al...