- All posts
- 8 Media Venture
- althetics
- aMMP8
- Annimari Korte
- Antibiotic resistance
- Apotek Härtat
- Aqua Dental
- athlete
- Award
- Baltics
- Bonnier
- Bonnier News
- Brain health
- Business
- Cancer
- cardiovascular disease
- caries
- Chemo therapy
- children
- collaboration agreement
- Croatia
- Denmark
- Denta
- Dental erosion
- Dentex
- diabetes
- Dual Light
- Duodecim
- EFP
- EFR
- Estonia
- EuroPerio
- event
- Expodental
- FIBO
- fund raising
- general health
- Gingivitis
- Gum disease
- HAP
- HealthHub Pharma
- HIDES
- Hospital infections
- hospital-acquired pneumonia
- IBD
- Iceland
- IDS COLOGNE
- implantology
- invest
- investment
- italy
- Koite Health
- Latvia
- Lithuania
- lumoral
- Lumoral App
- Lumoral Junior
- Maritime industry
- Media
- MegaGen
- Movie
- News
- Nordic markets
- Nordics
- O
- Olympics
- Oral health
- Oral hygiene
- Oral mucositis
- Patent
- PDT
- peri-implantitis
- Perio Master Clinic
- Periodontitis
- periodontology
- Photodynamic therapy
- Press
- Ranking
- Romania
- Scandinavian Society of Periodontology
- Science
- Seafarer
- Seedtable
- share issue
- Shareissue
- Siblings movie
- Space
- Spain
- spots
- Stroke
- Study
- sweden
- Tartar
- techtour
- Thailand
- UK
- United States
- Valentine's Day
- WHO
- World Cancer Day
- World Health Day
- World Heart Day
- world oral health day
- World Smile Day

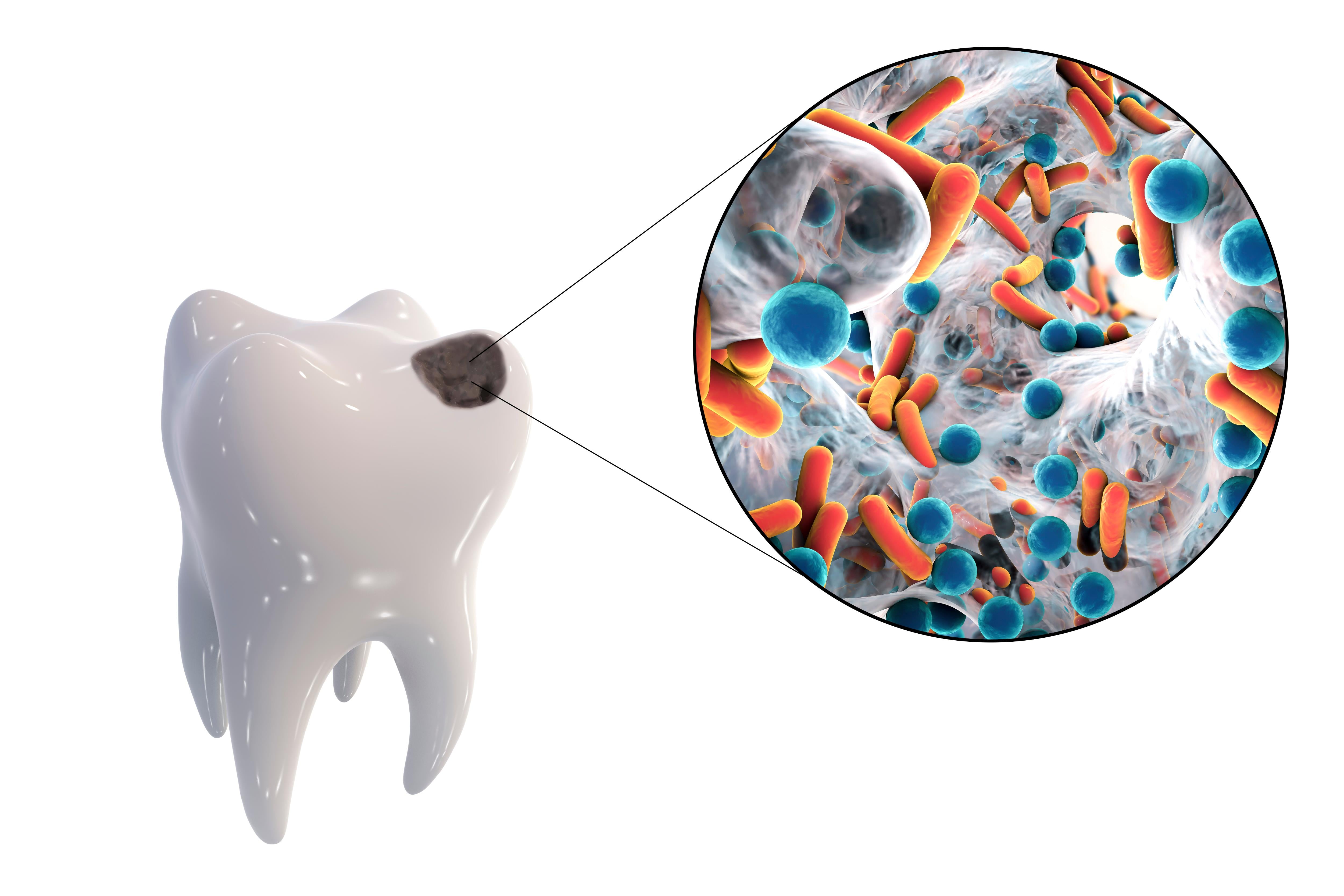
Thousands of Children Undergo Tooth Extractions Due to Tooth Decay in the UK
New figures from NHS England reveal that over 30,000 children and young people underwent hospital tooth extractions due to decay in the last year, The Oral Health Foundation reports. This marks a s...

Poor oral health can increase the risk of stroke
Every year, over 13 million people worldwide die from stroke. However, many of these incidents could be prevented through relatively simple means, such as a healthier diet, more exercise, or improv...

Oral Health and Brain Health: The Crucial Connection for Overall Well-being
Dental and oral bacteria have been linked to numerous chronic diseases throughout the body. Recent research indicates that thorough brushing and regular dental visits can also play a role in preven...
According to a report commissioned by the European Federation of Periodontology (EFP), 4.9 percent of global healthcare expenditure is allocated to treat preventable oral diseases such as gum infla...

Vegetarian Dental Care: Navigating Oral Health Challenges
Recent studies indicate that a vegetarian diet may increase the risk of tooth decay and erosion. The exact reasons for this are not fully understood, but several factors may contribute to it. Howev...

Lumoral: Significant steps in antibacterial oral care research
The Finnish oral care innovation Lumoral is of great interest to the academic world, and several new Lumoral studies have been launched in recent months. Koite Health Ltd’s Clinical Project Manager...