- All posts
- 8 Media Venture
- althetics
- aMMP8
- Annimari Korte
- Antibiotic resistance
- Apotek Härtat
- Aqua Dental
- athlete
- Award
- Baltics
- Bonnier
- Bonnier News
- Brain health
- Business
- Cancer
- cardiovascular disease
- caries
- Chemo therapy
- children
- collaboration agreement
- Croatia
- Denmark
- Denta
- Dental erosion
- Dentex
- diabetes
- Dual Light
- Duodecim
- EFP
- EFR
- Estonia
- EuroPerio
- event
- Expodental
- FIBO
- fund raising
- general health
- Gingivitis
- Gum disease
- HAP
- HealthHub Pharma
- HIDES
- Hospital infections
- hospital-acquired pneumonia
- IBD
- Iceland
- IDS COLOGNE
- implantology
- invest
- investment
- italy
- Koite Health
- Latvia
- Lithuania
- lumoral
- Lumoral App
- Lumoral Junior
- Maritime industry
- Media
- MegaGen
- Movie
- News
- Nordic markets
- Nordics
- O
- Olympics
- Oral health
- Oral hygiene
- Oral mucositis
- Patent
- PDT
- peri-implantitis
- Perio Master Clinic
- Periodontitis
- periodontology
- Photodynamic therapy
- Press
- Ranking
- Romania
- Scandinavian Society of Periodontology
- Science
- Seafarer
- Seedtable
- share issue
- Shareissue
- Siblings movie
- Spain
- spots
- Stroke
- Study
- sweden
- Tartar
- techtour
- Thailand
- UK
- United States
- Valentine's Day
- WHO
- World Cancer Day
- World Health Day
- World Heart Day
- world oral health day
- World Smile Day
According to a report commissioned by the European Federation of Periodontology (EFP), 4.9 percent of global healthcare expenditure is allocated to treat preventable oral diseases such as gum infla...

Revolutionizing Oral Mucositis Treatment: Antibacterial Light-Activated Therapy in Future Protocols
Oral mucositis, an inflammation of the oral mucosa, often occurs in association with cancer treatments, particularly radiation and chemotherapy. It manifests as severe pain, redness, and swelling i...

Antibacterial Dual-Light Therapy: A Novel and Effective Approach to Managing Oral Mucositis
Jessica Hentilä, a student at the Faculty of Medicine, University of Helsinki, conducted in-depth research on oral mucositis and its treatment. Oral mucositis is an inflammatory condition of the or...

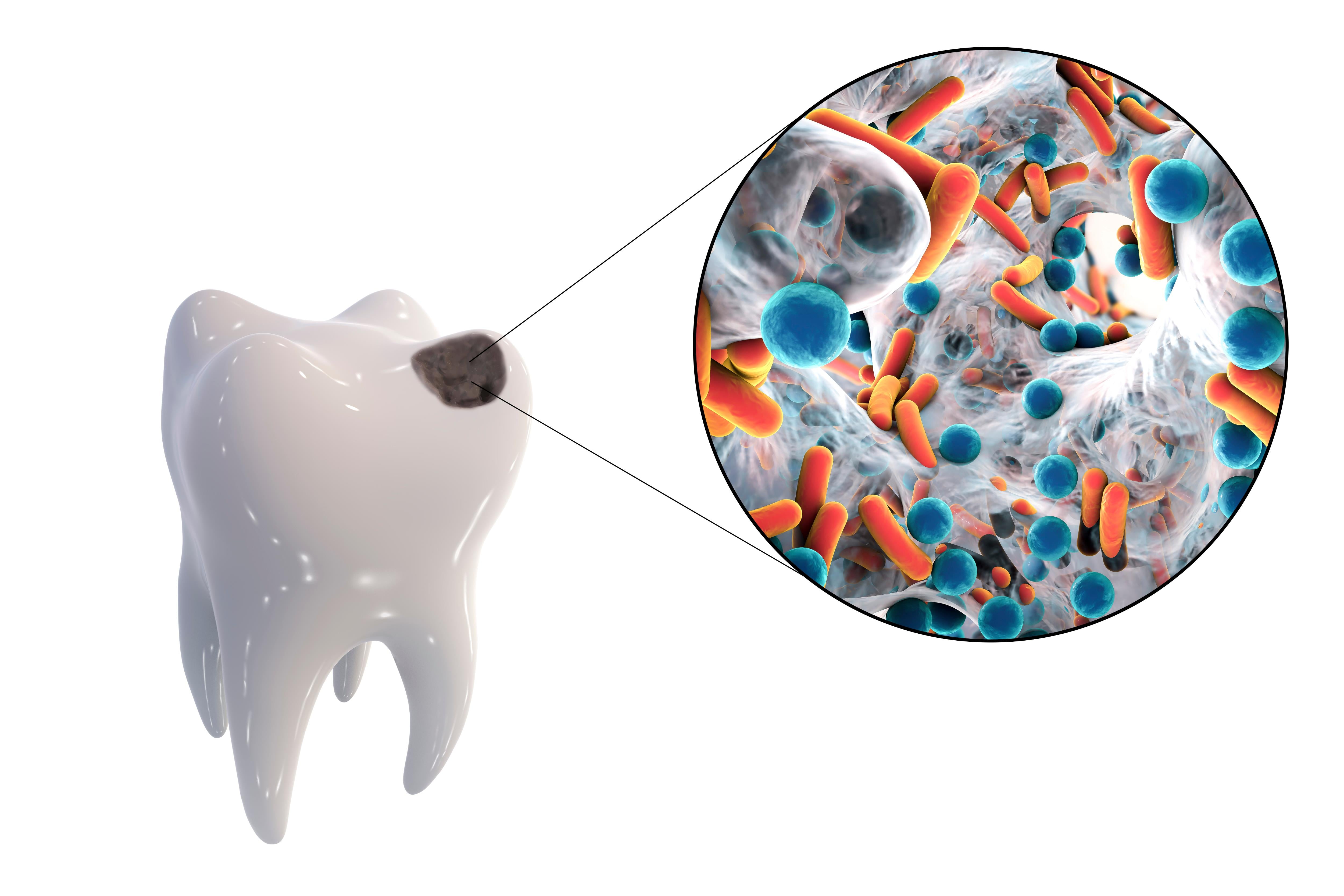
Poor Oral Health and Oral Dysbiosis: A Link to Systemic Diseases and Cancer
Scientists have discovered a significant link between poor oral health and systemic diseases, including specific cancers. This connection is centered around so-called oral dysbiosis, a condition wh...

“Siblings” brings the joys and sorrows of life close to its viewers
Finnish Director-writer Saara Cantell's film Sisarukset (Siblings) will premiere in Finnish cinemas on Friday, 27.10.2023. The film project was unique in its making, and the result is documentary-l...